Diabetic Retinopathy: The Silent Killer of Your Vision
Introduction Diabetic retinopathy is a serious eye condition that affects individuals with diabetes, leading to vision impairment and even blindness if left untreated. In this
Diabetic retinopathy is a serious eye condition that affects individuals with diabetes, leading to vision impairment and even blindness if left untreated. In this comprehensive guide, we will delve into the causes, symptoms, treatment options, prevention strategies, and real-life stories related to diabetic retinopathy to help you understand and manage this condition effectively
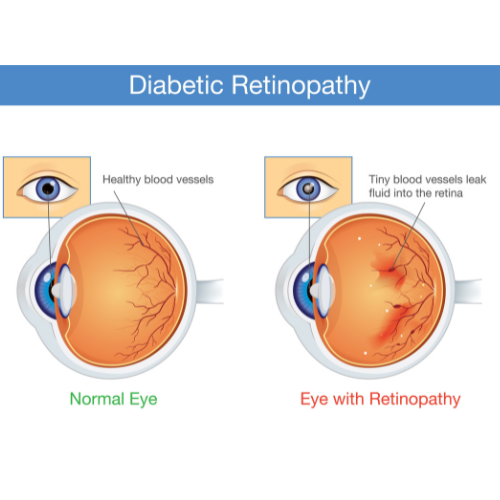
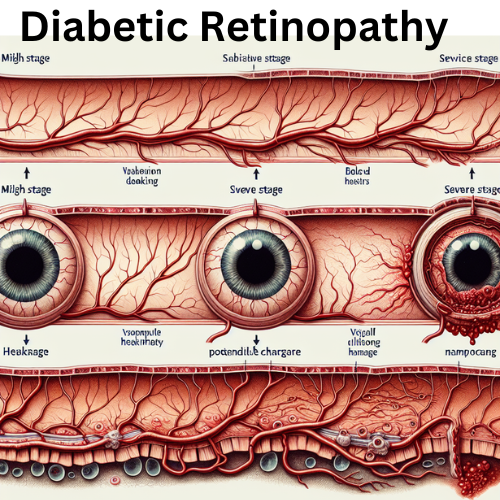
Diabetic retinopathy develops as a result of prolonged high blood sugar levels damaging the blood vessels in the retina. The condition progresses through different stages, starting with mild non-proliferative changes to more severe proliferative stages if left uncontrolled.
Common symptoms of diabetic retinopathy include blurred vision, floaters or dark spots in the vision, difficulty seeing at night, and sudden vision loss. Recognizing these signs early is crucial for prompt diagnosis and treatment.
Various treatment options are available to manage diabetic retinopathy, including laser treatment (photocoagulation), intraocular injections (anti-VEGF therapy), and vitrectomy surgery. These treatments aim to prevent further vision loss and preserve existing vision.
Preventing diabetic retinopathy involves effectively managing diabetes through lifestyle modifications, medication adherence, blood sugar control, and regular eye exams. By maintaining good overall health and eye care practices, individuals with diabetes can reduce their risk of developing diabetic retinopathy.
A Newsletter From Myo Clinic–
Anyone who has diabetes can develop diabetic retinopathy. The risk of developing the eye condition can increase as a result of:
Diabetic retinopathy involves the growth of abnormal blood vessels in the retina. Complications can lead to serious vision problems:
You can’t always prevent diabetic retinopathy. However, regular eye exams, good control of your blood sugar and blood pressure, and early intervention for vision problems can help prevent severe vision loss.
If you have diabetes, reduce your risk of getting diabetic retinopathy by doing the following:
Remember, diabetes doesn’t necessarily lead to vision loss. Taking an active role in diabetes management can go a long way toward preventing complications.
Discover inspiring real-life stories of individuals who have successfully managed diabetic retinopathy and maintained their vision health. These stories highlight the importance of early detection, treatment compliance, and proactive management of the condition to preserve vision and quality of life.
Diabetic retinopathy is a serious complication of diabetes that requires attention and proactive management to protect vision health. By understanding the causes, symptoms, treatment options, prevention strategies, and real-life examples related to diabetic retinopathy, individuals can take control of their eye health and make informed decisions to safeguard their vision for the future
Introduction Diabetic retinopathy is a serious eye condition that affects individuals with diabetes, leading to vision impairment and even blindness if left untreated. In this